Published online Aug 27, 2016. doi: 10.4240/wjgs.v8.i8.578
Peer-review started: March 25, 2016
First decision: May 17, 2016
Revised: May 23, 2016
Accepted: June 14, 2016
Article in press: June 16, 2016
Published online: August 27, 2016
Processing time: 154 Days and 22.1 Hours
To evaluate the utility of hand-assisted laparoscopic restorative proctocolectomy (HALS-RP) compared with the conventional open procedure (OPEN-RP).
Fifty-one patients who underwent restorative total proctocolectomy with rectal mucosectomy and ileal pouch anal anastomosis between January 2008 and July 2015 were retrospectively analyzed. Twenty-three patients in the HALS-RP group and twenty-four patients in the OPEN-RP group were compared. Four patients who had purely laparoscopic surgery were excluded. Restorative total proctocolectomy was performed with mucosectomy and a hand-sewn ileal-pouch-anal anastomosis. Preoperative comorbidities, intraoperative factors such as blood loss and operative time, postoperative complications, and postoperative course were compared between two groups.
Patients in both groups were matched with regards to patient age, gender, and American Society of Anesthesiologists score. There were no significant differences in extent of colitis, indications for surgery, preoperative comorbidities, and preoperative medications in the two groups. The median operative time for the HALS-RP group was 369 (320-420) min, slightly longer than the OPEN-RP group at 355 (318-421) min; this was not statistically significant. Blood loss was significantly less in HALS-RP [300 (230-402) mL] compared to OPEN-RP [512 (401-1162) mL, P = 0.003]. Anastomotic leakage was noted in 3 patients in the HALS-RP group and 2 patients in the OPEN-RP group (13% vs 8.3%, NS). The rates of other postoperative complications and the length of hospital stay were not different between the two groups.
HALS-RP can be performed with less blood loss and smaller skin incisions. This procedure is a feasible technique for total proctocolectomy for ulcerative colitis.
Core tip: This is a retrospective study to evaluate the utility of hand-assisted laparoscopic restorative proctocolectomy (HALS-RP) for ulcerative colitis (UC). Fifty-one patients underwent restorative proctocolectomy, and twenty-three patients in the HALS-RP were compared with twenty-four patients in the conventional open surgery group (OPEN-RP). The mean operative time for the HALS-RP group was not different to OPEN-RP group, but blood loss was significantly less in HALS-RP compared to OPEN-RP. HALS is a feasible procedure for restorative proctocolectomy for UC with small skin incision.
- Citation: Shimada N, Ohge H, Yano R, Murao N, Shigemoto N, Uegami S, Watadani Y, Uemura K, Murakami Y, Sueda T. Hand-assisted laparoscopic restorative proctocolectomy for ulcerative colitis. World J Gastrointest Surg 2016; 8(8): 578-582
- URL: https://www.wjgnet.com/1948-9366/full/v8/i8/578.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v8.i8.578
Laparoscopic surgery (LAP) was introduced in 1991 by Jacobs et al[1] for colorectal cancer, and is now the standard of care in many colorectal operations. Numerous studies have shown the benefits of LAP for colorectal cancer including less blood loss, less postoperative pain, earlier return of bowel function, and shorter length of hospital stay[2-4]. LAP for patients with ulcerative colitis (UC) was reported in 1992 by Peters[5], but it has not been widely accepted because of the complexity of the surgeries and long operative times[6]. Hand-assisted laparoscopic (HALS) was introduced in the mid-1990s as a hybrid technique[7]. Surgeons can provide direct retraction, perform the dissection, and control bleeding with one hand placed into the abdominal space through a small incision. HALS is a minimally invasive surgery and has been reported as an acceptable technique for total proctocolectomy (TPC). HALS is reported to be as minimally invasive as LAC[8], but there have been few reports comparing HALS and open surgery for UC. The aim of this study was to assess the utility of hand-assisted laparoscopic restorative proctocolectomy (HALS-RP) compared with the traditional open approach (OPEN-RP) performed by colorectal surgeons for patients with UC in a single institution.
A total of 95 patients underwent restorative TPC with mucosectomy and hand-sewn ileal-pouch anal anastomosis (IPAA) for UC in Hiroshima University Hospital from January 2008 to July 2015. Fifty-one patients who underwent a 2-staged procedure were included in this retrospective study. Those patients were divided into the HALS-RP group (n = 23) and the OPEN-RR group (n = 24) based on three surgeons’ preferences. Patients diagnosed with indeterminate colitis, or those who underwent pure laparoscopic surgery (n = 4), were excluded. Patient’s demographics, preoperative clinical information, intraoperative factors such as operative time and blood loss, postoperative complications, and postoperative course were compared. The patients were preoperatively categorized according to American Society of Anesthesiologists (ASA) classifications. Data are shown as the median with the interquartile range (IQR) in parentheses or means with standard deviations (SD) for continuous variables, and frequencies for categorical variables. Continuous data with a Gaussian distribution was showed as means and SD, and analyzed with the Student’s t test. In the case of a non-Gaussian distribution, continuous data were expressed as median and IQR and analyzed with the Wilcoxon rank-sum test. For categorical variables, the Pearsons χ2 test was performed, and Fisher’s exact test was used when the data set was small (expected cell counts were < 5). A P value < 0.05 was considered statistically significant. Statistical evaluation was carried out using the JMP version11 software (SAS institute Japan).
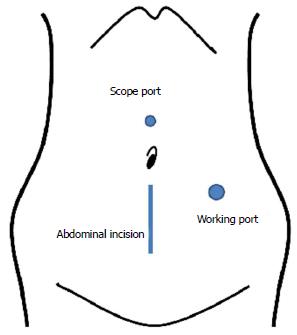
Transanal mucosectomy was performed in the jack-knife position. During this procedure, the anterior wall of the rectum was separated from the prostate gland or vaginal wall. The posterior wall of the rectum could be separated from the sacrum via transmesorectal excision. Patients were then placed in the lithotomy position. A 7-cm vertical incision below the umbilicus was made for the hand port and the wound protector was inserted. Mobilization of the right side colon and sigmoid colon was performed, and the terminal ileum was resected through the small incision under direct vision. Two trocars were placed in the upper umbilical region for the laparoscope and the left mid-abdomen for the surgeon’s right hand (Figure 1). A hand-assist device (Gel Port® system) was assembled within the wound protector. Pneumoperitoneum was initiated and the greater omentum was dissected from the transverse colon. The left colon including the splenic flexure was mobilized, and the mesentery was divided outside of the marginal artery of colon. A vessel sealing system (LigaSure®; Valleylab) was used for this purpose. After pneumoperitoneum, mobilization of the rectum was performed through the incision. A J-pouch was constructed at the terminal ileum with linear staplers, and hand-sewn to the anal verge.
Twenty-three cases in the HALS-RP group and 24 cases in the OPEN-RP group were matched in regards to patient age, gender, and ASA score (Table 1). However, body mass index (BMI) in the HALS-RP was 20.8 ± 3.1, which was significantly less than that of the OPEN-RP group (22.6 ± 3.3, P = 0.043). There were no significant differences in extent of colitis, indications for surgery, preoperative comorbidities, and preoperative medications in the two groups. Preoperative leukocyte count was higher in the HALS-RP group than OPEN-RP group (7486 ± 478 vs 5661 ± 410, P = 0.002). The amount of total-corticosteroid and C-reactive protein was also higher than the OPEN-RP group; this was not significantly different.
| HALS-RP (n = 23) | OPEN-RP (n = 24) | P value | |
| Age, mean | 42.7 ± 12.7 | 50.9 ± 18.1 | NS |
| Sex (male/female) | 15/8 | 18/6 | NS |
| BMI, kg/m2 | 20.8 ± 3.1 | 22.6 ± 3.3 | 0.043 |
| ASA score | NS | ||
| 1 | 1 (4.3) | 1 (4.2) | |
| 2 | 22 (95.7) | 23 (95.8) | |
| 3 | 0 (0) | 0 (0) | |
| Disease duration (month, median) | 132 (66-216) | 136 (36-256) | NS |
| Extent of colitis | NS | ||
| Pancolitis | 17 (73.9) | 16 (76.1) | |
| Left side colitis | 6 (26.1) | 4 (19.0) | |
| Rectal colitis | 0 (0) | 1 (4.8) | |
| Indication for surgery | NS | ||
| Cancer/dysplasia | 6 (26.9) | 10 (41.6) | |
| Stricture | 4 (17.4) | 2 (8.33) | |
| Refractory to medication | 13 (56.5) | 10 (41.6) | |
| Others | 0 (0) | 2 (4.26) | |
| Preoperative medication | |||
| Corticosteroid (mg, median) | 4400 (1000-8700) | 950 (0-4462) | NS |
| 12 (50%) | |||
| L-CAP/G-CAP | 10 (434) | 12 (50) | NS |
| CyA, Tarolimus | 3 (8.7) | 0 (0) | NS |
| Biologics | 2 (8.7) | 3 (12.5) | NS |
| Preoperative comorbidity | NS | ||
| HT | 3 (13) | 4 (16.7) | |
| DM | 1 (4.3) | 3 (12.5) | |
| Preoperative laboratory data (average ± SD) | |||
| Leukocyte | 7486 ± 478 | 5661 ± 410 | 0.002 |
| Hemoglobin | 11.8 ± 0.74 | 13.05 ± 0.28 | NS |
| Serum albumin | 3.96 ± 0.11 | 4.16 ± 0.221 | NS |
| CRP | 1.42 ± 0.749 | 0.29 ± 0.104 | NS |
The operative outcomes and complications are summarized in Table 2. The mean operative time for the HALS-RP group was slightly longer, but this was not significantly different [HALS-RP 369 (320-420) min vs OPEN-RP 355 (318-421) min]. Blood loss was significantly lower in the HALS-RP group (300 (230-402) mL vs 512 (401-1162) mL, P = 0.003). IPAA anastomotic leakage was noted in 3 patients in the HALS-RP group and 2 patients in the OPEN-RP group (13% vs 8.3%, NS). Rates of surgical site infection were not significantly different. Superficial and deep surgical site infections developed in 3 cases in the HALS-RP group (13.0%) and 3 cases in the OPEN-RP group (12.4%, NS). Organ space infections were noted in 5 cases in the HALS-RP group (21.7%) and 4 in the OPEN-RP group (16.7%, NS). Other postoperative complications such as small bowel obstruction, venous thrombosis, and neurologic bladder dysfunction were also similar.
| HALS-RP (n = 23) | OPEN-RP (n = 24) | P value | |
| Surgical outcome | |||
| Operation time (min, median) | 369 (320-420) | 355 (318-421) | NS |
| Blood loss (mL, median) | 300 (230-402) | 512 (401-1162) | 0.003 |
| Bowel movement (d, mean) | 1.5 ± 0.13 | 1.8 ± 1.4 | NS |
| Toleration of liquids | 1.3 ± 0.13 | 1.29 ± 1.75 | NS |
| Toleration of solid diet | 5.26 ± 0.75 | 3.62 ± 0.29 | NS |
| Length of stay (d) | 20 (16-26) | 18 (14-29) | NS |
| Complications, n (%) | |||
| IPAA anastomotic leak | 3 (13.04) | 2 (8.33) | NS |
| Surgical site infection | |||
| Superficial wound infection | 3 (13.04) | 1 (4.17) | NS |
| Deep wound infection | 0 (0) | 2 (8.3) | NS |
| Organ space infection | 5 (21.7) | 4 (16.67) | NS |
| Small bowel obstruction | 6 (26.0) | 4 (16.6) | NS |
| Venous thromboembolism | 2 (8.7) | 3 (6.38) | NS |
| Neurogic bladder dysfunction | 0 (0) | 1 (4.17) | NS |
| Hemorrhage | 0 (0) | 1 (4.17) | NS |
Return of bowel function, which was estimated by bilious output from the ileostomy, was similar between the two groups (1.5 ± 0.13 d and 1.8 ± 1.4 d, P = 0.26). Tolerance of liquid diet was 1.3 ± 0.13 d and solid diet was 5.26 ± 0.75 d in the HALS-RP group; these were similar to the OPEN-RP group (1.29 ± 1.75 d and 3.62 ± 0.29 d). The length of hospital stay after surgery was not different between the two groups 20 (16-26) d in HALS-RP, 18 (14-29) d in OPEN-RP, P = 0.408.
Laparoscopic surgery is common practice in segmental resection for colorectal disease namely because it provides a good field of view in the abdominal cavity.Furthermore, smaller skin incisions and faster recovery of bowel function are achieved using this technique. However, laparoscopic TPC for patients with UC is still not widely accepted as it is a longer and more complex surgery, and difficult to handle inflamed bowel laparoscopically without causing injury. In terms of avoidance of bowel edema, shorter operative times are preferred for ileal-pouch and anal anastomosis healing. On the other hand, patients with UC are relatively young and often prefer small skin incisions for cosmetic reasons. Recently, HALS for colorectal surgery was compared with conventional LAP, and showed that a HALS approach shortened operative time, but overall morbidity, time to return of bowel function, and length of hospital stay were similar to those of LAP[8-10]. While we adopted HALS in 2008, there have been few studies comparing it with traditional open surgery for TPC with mucosectomy. In this study, we aimed to compare HALS-RP and traditional open surgery over the last 8 years in a single institution.
In terms of operative time, one study showed that HALS reduced time by 33 min in sigmoid/left colectomy, and 57 min in total colectomy compared with a conventional LAP technique[9]. Aalbers et al[11] reported that the most important advantage of HALS in TPC was reduction in operating time, making the operation more efficient. In our series, HALS-RP was successfully completed without significant increase of operative time compared with OPEN-RP. Operative time of 374 min in this study series was still longer than previous studies, which reported times ranging from 210 to 356 min[6,12-15]. We speculate that this was because we started the trans-anal procedure with a mucosectomy in the jack-knife position and the time required for position change to modified lithotomy position was included. All told, this was approximately 70 min before the abdominal incision. Moreover, we chose a hand-sewn IPAA for all cases, which takes longer than a stapled IPAA, the most common technique reported in previous studies. HALS-RP showed significantly less blood loss than OPEN-RP. We attribute this to the good view of the splenic flexure as compared to that with open surgery.
Nakajima et al[14] reported that HALS maintains the early postoperative benefit of minimally invasive surgery as well as a totally laparoscopic approach for TPC. However, we are of the opinion that a HALS approach may hasten return of bowel function given there is direct manipulation of the intestine with the operator’s hand. Accordingly, in this study, an advantage of the return of postoperative bowel function in the HALS-RP group was not shown. The median length of hospital stay in this study was also the same in both groups [20 (16-26) d in HALS-RR, 18 (14-29) d in OPEN-RP]. Although both were longer than in other studies[6,14], diet advancement was done in a traditional step-wise fashion, and time was devoted to patient education regarding ileostomy care and medical control of diarrhea.
Total length of skin incisions for HALS-RP at our institution was 8 cm, with a 7-cm midline incision, and two 0.5 cm incisions for trocars. Laparoscopic TPC uses a total incision length of 4.1 to 8.2 cm for trocars and construction of the ileal-pouch[11,13]. Thus, regarding total skin incision length, there are few cosmetic advantages of totally laparoscopic TPC.
Currently we use three different approaches for TPC: Open surgery, HALS, and LAP. Choice of technique is tailored to the individual patient. For young women, LAP may be appropriate. For patients with prior surgery, open surgery should be considered. HALS has the benefit of having the view of laparoscopic surgery but the time saving of open surgery, which may reduce surgeon stress.
This study has several limitations. Our case numbers are small. This is a nonrandomized comparison between two groups in a retrospective fashion. Surgical methods were not selected in accordance with any definitive criteria, but rather by surgeons’ preferences, which could introduce some element of bias.
HALS for TPC affords the good operative view of laparoscopic surgery as well as the tactile feedback of open surgery. It is an acceptable alternative to conventional open surgery.
Total proctocolectomy (TPC) with mucosectomy for patients with ulcerative colitis (UC) is a complex, lengthy procedure. Traditional laparoscopic surgery (LAP) for UC has taken long operation time. The authors hypothesize that hand-assisted laparoscopic restorative proctocolectomy (HALS-RP) is superior to LAP for this disease.
Although some study report about HALS-RP compared with LAP, there have been few studies comparing it with traditional open surgery for TPC.
This study indicated that HALS-RP is acceptable with less blood loss, and without increase of operative time and postoperative complications compared with open procedure (OPEN-RP).
HALS-RP is useful technique for TPC for UC with small skin incision and affords the operative good view.
This is a retrospective single-center study. Twenty-three patients in the HALS-RP group and 24 cases in the OPEN-RP group were matched in regards to patient age, gender, and anesthesiologists score. The study demonstrates that the rates of other postoperative complications and the length of hospital stay were not different between the two groups, with less blood loss and smaller skin incisions in the HALS-RP group.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Korelitz BI, Manguso F S- Editor: Qi Y L- Editor: A E- Editor: Wu HL
| 1. | Jacobs M, Verdeja JC, Goldstein HS. Minimally invasive colon resection (laparoscopic colectomy). Surg Laparosc Endosc. 1991;1:144-150. [PubMed] |
| 2. | Lacy AM, García-Valdecasas JC, Delgado S, Castells A, Taurá P, Piqué JM, Visa J. Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet. 2002;359:2224-2229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1901] [Cited by in RCA: 1810] [Article Influence: 78.7] [Reference Citation Analysis (0)] |
| 3. | Laparoscopically assisted colectomy is as safe and effective as open colectomy in people with colon cancer Abstracted from: Nelson H, Sargent D, Wieand HS, et al; for the Clinical Outcomes of Surgical Therapy Study Group. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 2004; 350: 2050-2059. Cancer Treat Rev. 2004;30:707-709. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 43] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Påhlman L, Cuesta MA, Msika S. Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol. 2005;6:477-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1691] [Cited by in RCA: 1666] [Article Influence: 83.3] [Reference Citation Analysis (0)] |
| 5. | Peters WR. Laparoscopic total proctocolectomy with creation of ileostomy for ulcerative colitis: report of two cases. J Laparoendosc Surg. 1992;2:175-178. [PubMed] |
| 6. | Rivadeneira DE, Marcello PW, Roberts PL, Rusin LC, Murray JJ, Coller JA, Schoetz DJ. Benefits of hand-assisted laparoscopic restorative proctocolectomy: a comparative study. Dis Colon Rectum. 2004;47:1371-1376. [PubMed] |
| 7. | Ou H. Laparoscopic-assisted mini laparatomy with colectomy. Dis Colon Rectum. 1995;38:324-326. [PubMed] |
| 8. | Pyo DH, Huh JW, Park YA, Cho YB, Yun SH, Kim HC, Lee WY, Chun HK. A comparison of hand-assisted laparoscopic surgery and conventional laparoscopic surgery in rectal cancer: a propensity score analysis. Surg Endosc. 2016;30:2449-2456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Marcello PW, Fleshman JW, Milsom JW, Read TE, Arnell TD, Birnbaum EH, Feingold DL, Lee SW, Mutch MG, Sonoda T. Hand-assisted laparoscopic vs. laparoscopic colorectal surgery: a multicenter, prospective, randomized trial. Dis Colon Rectum. 2008;51:818-826; discussion 826-828. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 120] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 10. | Yang I, Boushey RP, Marcello PW. Hand-assisted laparoscopic colorectal surgery. Tech Coloproctol. 2013;17 Suppl 1:S23-S27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Aalbers AG, Doeksen A, Van Berge Henegouwen MI, Bemelman WA. Hand-assisted laparoscopic versus open approach in colorectal surgery: a systematic review. Colorectal Dis. 2010;12:287-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 46] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 12. | Polle SW, van Berge Henegouwen MI, Slors JF, Cuesta MA, Gouma DJ, Bemelman WA. Total laparoscopic restorative proctocolectomy: are there advantages compared with the open and hand-assisted approaches? Dis Colon Rectum. 2008;51:541-548. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 30] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Tsuruta M, Hasegawa H, Ishii Y, Endo T, Ochiai H, Hibi T, Kitagawa Y. Hand-assisted versus conventional laparoscopic restorative proctocolectomy for ulcerative colitis. Surg Laparosc Endosc Percutan Tech. 2009;19:52-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Nakajima K, Lee SW, Cocilovo C, Foglia C, Sonoda T, Milsom JW. Laparoscopic total colectomy: hand-assisted vs standard technique. Surg Endosc. 2004;18:582-586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 63] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 15. | Nakajima K, Nezu R, Ito T, Nishida T. Hand-assisted laparoscopic restorative proctocolectomy for ulcerative colitis: the optimization of instrumentation toward standardization. Surg Today. 2010;40:840-844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |